As a non-invasive way that is widely applicable in various environments, POCUS is now replacing stethoscopes in emergency departments, which provides a more intuitive description of the functions and status of key parts, effectively improving the efficiency of diagnosis and treatment of emergency patients, and reducing costs, complication rates and mortality. With the continuous development and advancement of ultrasound miniaturization technology, ultrasound is no longer limited to professional imaging physicians. After training, physicians in various clinical departments have begun to use wireless pocket ultrasound to visualize conditions for diagnosis and treatment.
Transthoracic Echocardiography (TTE) Window
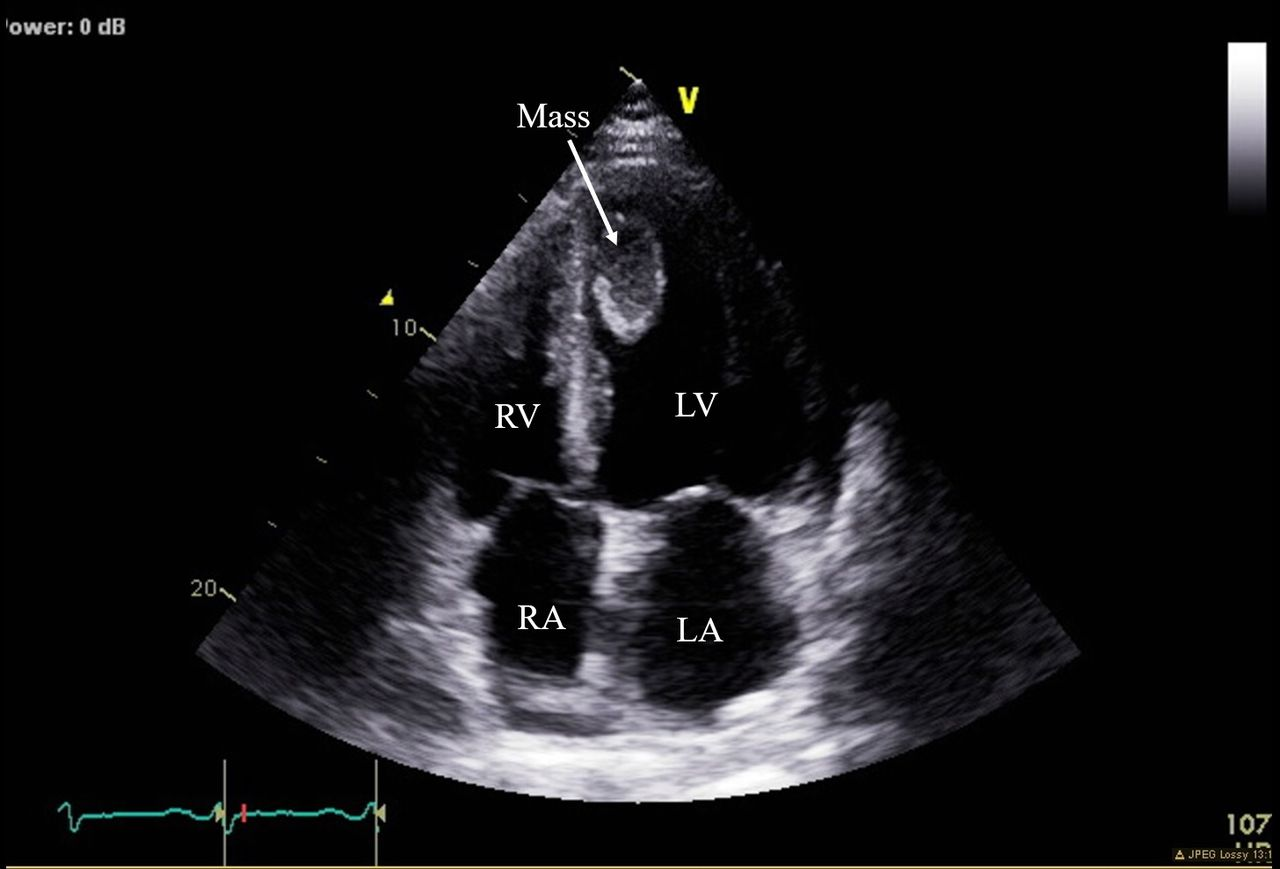
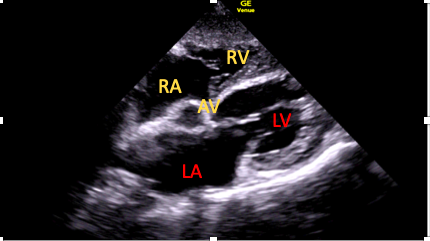
Transthoracic echocardiography (TTE) is an important breakthrough in non-invasive observation of cardiac anatomy. The heart has 4 chambers: right atrium, right ventricle, left atrium, and left ventricle. They are separated by their respective valves: tricuspid valve (TV), pulmonary valve leaflets (PVL), mitral valve (MV), and aortic valves (AV). These structures are clearly visible through the four main cardiac ultrasound views (acoustic windows).
The four acoustic windows of echocardiography are parasternal, apical, subcostal, and suprasternal. Next, let’s take a look at the cardiac ultrasound images that can be obtained in these four acoustic windows.
Parasternal window
1 .Parasternal Long Axis View(PLAX View)
The long-axis view of the left ventricle can measure most chamber size parameters, such as evaluating Ejection Fraction (EF), Blood Vessel Width, Left Atrium Diameter (LAD), left ventricular end-diastolic diameters (LVDd), etc. In addition, this view is the standard view for M-mode ultrasound scanning, which is used to measure the diameter of the heart and great vessels and determine whether the cardiac chambers and great vessels are normal.
After the patient lies on the left side, place the probe between the 3rd and 4th ribs on the left edge of the sternum and make the mark point of the ultrasound probe facing the patient’s right shoulder. At this time, the sound beam emitted by the probe is parallel to the line connecting the patient’s right shoulder to the left rib, and the obtained image is equivalent to that seen when the left ventricle of the heart is cut along its long axis.
After using pocket ultrasound to scan the image, physicians first need to observe the heart’s basic structures: myocardium, valves, and pericardium. In the image, the aorta is seen on the right, the apex of the heart on the left, the chest wall and right ventricle in front, and the posterior wall structures behind. After determining the optimal parasternal long-axis image, imaging depth should be adjusted to visualize the structures of the pericardial and evaluate for pleural or the degree of pericardial effusion.
Secondly, observe the size of the left and right ventricles under ultrasound screening. If the left ventricle is full in shape, consider whether is left ventricular hypertrophy; if the movement of the interventricular septum becomes flat or even convex to the left ventricular side, it shows that the anterior ventricular septum and the posterior wall of the left ventricle move in the same direction. If the right ventricle is full, consider whether is right ventricular hypertrophy.
Finally, enlarge the image to observe the aortic root and aortic valve. The aortic valve is mainly observed for calcification, vegetation, and prolapse; whether there is stenosis above and below the valve; whether there is dilatation, intimal plaque, and dissection of the aorta. Also need to observe the leaflet shape and activity of the mitral valve (MV), whether there are calcifications, vegetations, prolapse, and subvalvular devices (chordae tendineae, papillary muscles).
2. PARASTERNAL SHORT AXIS VIEWS (PSAX Views)
The parasternal short-axis view is the best view for observing left ventricular size, wall motion, myocardial motion and contractility.
Place the ultrasound probe between the 3rd and 4th ribs on the left edge of the sternum. Rotate the probe clockwise so that the sound beam is perpendicular to the long-axis section of the left ventricle. At this time, the mark point of the ultrasound probe points to the left shoulder and the sound beam is parallel to the line connecting the left shoulder to the right rib. Therefore, the following short-axis section images can be obtained respectively: apex level, mitral valve level, and great vessel level.
• Parasternal short-axis – mitral valve (PSAX-MV)
After putting the probe directly perpendicular to the chest wall, the sound beam transects the left ventricle at the level of the mitral valve. The cross-section of the anterior mitral valve leaflet (AMVL) and posterior mitral leaflet (PML) can be observed. This view mainly shows right ventricular anterior wall (RVAW), right ventricular cavity, left ventricular cavity, mitral valve and left ventricular anterior wall, septum (anterior septum and inferior septum), inferior wall, and lateral wall (inferolateral wall and anterolateral wall), pericardium and other important cardiovascular structures.
Since the sound beam is almost perpendicular to most of the left ventricular wall at this time, the mitral valve is very important for evaluating the left ventricular wall and left ventricular chamber which is commonly used for measuring left ventricular wall thickness and thickening rate, cardiac function measurement indicators, etc.
Reference values for absolute echocardiographic measurements
LV end diastolic dimension 39–56.5 mm
LV end systolic dimension 23–38 mm
Posterior wall thickness at end diastole 6–11 mm
Septal thickness at end diastole 6–11mm
•Parasternal Short Axis (PSAX)
After obtaining the cross-section of the left ventricle at the level of the mitral valve, tilt the probe downward toward the apex to obtain a cross-section of the left ventricular apex, or the probe can be directly placed on the apex pulse point. This view is mainly used to evaluate the wall motion of the left ventricular apex and to observe apical thrombus, apical aneurysm, apical hypertrophy, etc.
•Level of large vessel
Continue to tilt the probe upward to obtain a transverse section of the aorta. The right ventricle (RV), right ventricular outflow tract (RVOT), main pulmonary artery (MPA), aorta, and three aortic valves can be observed. Sometimes, the left coronary artery (LCA) and the right coronary artery (RCA) can also be observed at the aortic opening at the opening of the right coronary artery.
The level of the great vessels is one of the best views to observe the aortic root. When the heart function is normal, the aorta is round, and the three aortic valve leaves are Y-shaped during diastole. The right ventricular outflow tract (RVOT) surrounds the aorta and is located in front of the aorta from left to right. It is located in front of the circular aorta in cross-section, and the pulmonary valve is in front of the right side of the aorta.
•Level of papillary muscle
Based on the left ventricle’s short-axis mitral valve horizontal section, tilt the probe toward the apex to obtain the short-axis papillary muscle horizontal section of the left ventricle. This view is often used to observe the position, thickness, overall structure, and segmental motion of the ventricular septum and left ventricular wall, and to observe the shape, inner diameter, intracavity structure, and function of the left ventricular cavity. It is a commonly used ultrasound section to evaluate coronary heart disease.
The papillary muscle level section can also be used to calculate the endocardium to obtain the LV end-diastolic area (LVEDA). However, it is worth noting that this level cannot be measured for the patient who suffers from concentric hypertrophy or abnormal ventricular wall motion.
3.ParasternalLong-Axis View(PLAX View)
•A4C View
After the patient is placed in the left lateral decubitus position, put the ultrasound probe at the apical pulse, or near the maximum pulse point, and the sound beam is directed upward and slightly toward the patient’s right scapula to obtain an apical four-chamber view (A4C). In standard A4C, the interventricular septum (IVS) is seen perpendicular to the center of the screen, with the apex above and the atria at the bottom. The mitral valve (MV) and tricuspid valve (TV) can be seen throughout the cardiac cycle, and there is no axial contraction movement of the apex.
The A4C view is a very important view in echocardiography. The position of the left and right ventricles and the atrioventricular connection relationship can be determined by identifying the atrioventricular valves and regulatory bundles. The healthy right ventricle (RV) is triangular in the apical four-chamber view. The end-diastolic area of the right ventricle is less than 2/3 of the left ventricle, and the interventricular septum is completely convex toward the right ventricle. Normally, the end-diastolic area of the right ventricle ( (RVED area) /the end-diastolic area of the left ventricle (LVED area) is <0.6. If the ratio is greater than 1, it can be diagnosed as severe dilation.
•Simpson method to measure left ventricular ejection fraction (EF)
Left ventricular ejection fraction (LVEF) measurement is one of the methods to quantitatively evaluate left ventricular systolic function. Common measurement methods include M-mode ultrasound measurement, Simpson method, etc. The 2015 ASE guidelines recommend the biplane disk summation method (Simpson method) for left ventricular volume measurement, and also clearly state that 2D measurement to obtain left ventricular volume is no longer recommended.
The correct measurement method is: after obtaining a clear and accurate apical four-chamber view (A4C), use the trackball to trace the left ventricular endocardial edge during left ventricular end diastole and end systole which includes papillary muscles and trabeculae. After tracing and calculating the intima, measure the length of the cardiac chamber from the plane of the mitral annulus to the apex. Calculating the left ventricular end-diastolic and end-systolic volumes according to the following formula.
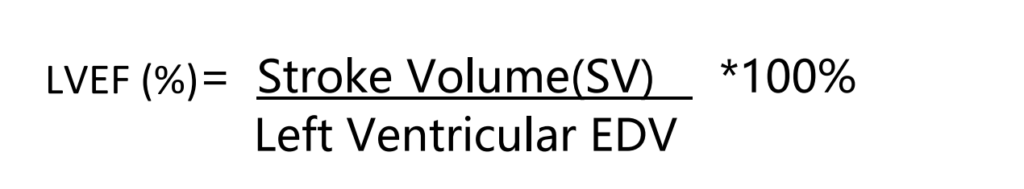
The Simpson method is suitable for left ventricular cavities of any shape, can calculate various irregular-shaped left ventricular cavities, and has a good fit for conditions such as heart failure, left ventricular wall dyskinesia, and ventricular aneurysm. However, the Simpson method has high requirements for image quality, which needs a clear four-chamber cardiac section and complete endocardial tracing. Therefore, calculated EF has high requirements for the proficiency and professionalism of ultrasound users. Viatom C10 ultrasound is specially designed for echocardiography, the unique heart probe and preset mode can quickly scan accurate heart chamber images even for beginners.
•Apical five-chamber view (A5C)
By tilting the probe upward in the A4C view, the lof ventricular outflow tract (LVOT) and proximal aortic root can be observed in the center of the image of the four-chamber heart section, and the A5C view can be obtained. At this time, the handheld ultrasound beam is nearly parallel to the blood flow of the LVOT and AV, so the apical five-chamber view is mainly used to evaluate the blood flow of the LVOT and AV.
Color Doppler Flow Imaging (CDFI): If the pulse Doppler sampling frame is placed on the AV, the forward blood flow spectrum of the AV can be obtained. Normally the blue blood flow through the AV during systole is most noticeable in the center and becomes darker near the wall.
If aortic valve stenosis, it shows that the blood flow in the LVOT during systole accelerates at the proximal end of the valve orifice to form a colorful mosaic of jet beams. The width of the jet beam is inversely proportional to the degree of stenosis. The transvalvular pressure difference can be calculated by measuring the flow velocity of the aortic valve orifice with continuous wave Doppler, and the average pressure difference can reflect the severity of aortic valve stenosis.
| Degree of stenosis | Valve morphology | Maximum pressure difference(mmHg) | Average pressure difference(mmHg) |
| Mild | Thickened valve leaflets and limited movement | 16-50 | <25 |
| Moderate | Thickened leaflets and reduced movement | 50-80 | 25-50 |
| Severe | The valve leaflets are significantly thickened and movement is significantly restricted. | >80 | >50 |
However, it is worth noting that if the patient is accompanied by left ventricular systolic dysfunction (LVSD), left ventricular hypertrophy (LVG), hypertension, aortic regurgitation, etc., the evaluation results will be affected.
4.Subcostal Window
When the parasternal acoustic window is unavailable, subcostal cardiac imaging may be preferred. The subcostal window is mainly used to evaluate the pericardium, right ventricular, and large abdominal vessels such as the superior vena cava, inferior vena cava, the right ventricle (RV) free wall and RV thickness and hepatic veins.
Place the probe in the midline of the heart or slightly to the right, with the mark point of the ultrasound probe facing downward toward the patient’s spine. The liver, hepatic vessels, and inferior vena cava can be observed when the probe is tilted downward and slightly toward the patient’s right side. The probe is slightly upward, and the hepatic vein can be seen flowing into the inferior vena cava. By rotating the probe so that the groove faces the patient’s right rib, the long axis of the inferior vena cava can be recorded, and color flow images and pulsed Doppler can record the blood flow in the hepatic artery.
•Subcostal Four-Chamber View
Tilt the probe upward to the pointed between the suprasternal fossa and the left clavicle of the patient, and images of the four parasternal cardiac chambers can be obtained. This section can display the left and right ventricles, left and right atria, pericardium and left lobe of the liver. The left and right ventricles are located on the left side of the image, and the left and right atria are located on the right side of the image.
The subxiphoid four-chamber view is the best view for observing pericardial effusion and cardiac movement during cardiopulmonary resuscitation.
The Subcostal Four-Chamber View remains the choice for screening to assess the possibility of PH and to evaluate RV function. Under the SC window, because the ultrasound beam is perpendicular to each septum at this time, atrial septal defect (ASD), ventricular septal defect (VSD), and RV wall thickness can be evaluated through this section. The normal value of right ventricular wall (RVWT) is ≤0.5cm. When the end-diastolic thickness exceeds 0.5cm, RV hypertrophy can be initially diagnosed.
5.Suprasternal Window
Place the probe in the suprasternal fossa with the long axis of the probe toward the left, parallel to the trachea, and the mark point of the ultrasound probe facing toward the right clavicle area. The suprasternal window shows the deep aorta, the origin of the aortic arch, and the descending aorta. Occasionally, aortic valve leaflets may be observed in the aortic root.
In the suprasternal view image, the deep aorta is on the left, the descending aorta is on the right, the short axis of the right pulmonary artery is behind the deep aorta, below the aortic arch, and below the right pulmonary artery is the left atrium. However, the suprasternal fossa acoustic window is not suitable for patients with chronic obstructive pulmonary disease and emphysema to diagnosis cardiac because the patient’s lungs are too inflated to observe the above structures.
•Aortic dissection
The long-axis view of the aortic arch in the suprasternal fossa has important diagnostic value in aortic dissection. There are two main classifications of aortic dissection, namely the DeBakey classification and the Standford classification, these two classifications are both based on the location and extent. Therefore, the aorta, aortic arch and descending aorta are under ultrasound scanning The initial part is the necessary basis for classification diagnosis.
- In the DeBakey classification, Type I means the breach is located in the ascending aorta or aortic arch, and the hematoma involves the entire ascending aorta, aortic arch, and descending aorta; Type II means the breach is located in the ascending aorta and is limited to the ascending aorta; Type III, the breach is located distal to the left subclavian artery, involving the thoracic aorta (IIIa) or abdominal aorta (IIIb).
- In the Stanford classification, type A, aortic dissection involves the ascending aorta; type B, aortic dissection only involves the descending aorta.
If the patient has obvious chest pain symptoms and the parasternal section has shown widening of the ascending aorta or thoracic aorta, attention should be paid to scanning the entire aorta during the long-axis section of the aortic arch, including the parasternal, suprasternal fossa, and subcostal aorta, abdomen and even thighs, try to exclude artifacts in the aorta.

Bedside Echocardiography
Bedside cardiac ultrasound is to use wireless ultrasound or pocket ultrasound to conduct a qualitative assessment of the heart. Ordinary physicians can operate it after receiving basic training in simple transthoracic echocardiography (TTE), which is commonly used in emergency departments and critical care departments for rapid clinical examination methods.
Bedside cardiac ultrasound in emergency departments
Emergency department patients often present with serious and complex conditions such as trauma, coma, chest pain, abdominal pain, etc. It is very important to ensure that patients can receive treatment within the golden time, so fast and accurate diagnostic methods are important for emergency departments.
Bedside echocardiographic assessment for trauma
Common trauma is blunt injury, and some blunt injuries can cause intra-abdominal bleeding and cause hypovolemic shock. Traditional trauma identification methods include DPL and CT, but their invasiveness and high time cost make the above two methods unable to meet the needs of rapid emergency diagnosis of trauma types.
The noninvasiveness, ease of use, and timeliness of bedside echocardiography have significantly impacted the assessment and treatment of external trauma. FAST (focused assessment with sonography for trauma) is an ultrasound solution for rapid assessment of patients with acute chest and abdominal closed injuries in emergency departments. After a large number of experiments, it has been proven that the specificity of FAST can reach 98-100%. It has been included in the Advanced Trauma Life Support (ATLS) protocol and has become a necessary step in acute trauma examination.[1]
Emergency physicians can use wireless handheld ultrasound to complete the FAST exam in five minutes. Usually, a convex array probe is used to scan under the xiphoid process, right abdomen, left abdomen, and pelvis to check whether free gas and liquid is overflowing due to organ damage in the perihepatic, perisplenic, pericardium, and other parts. The results of FAST are of great significance to whether emergency laparotomy or exploratory thoracotomy is performed.
Bedside echocardiographic assessment for shock management
Bedside ultrasound has become the tool of choice for emergency critical illness diagnosis. Although the factors of shock are increasingly diverse and complex, the use of wireless ultrasound for examination means that there is no need for invasive hemodynamic assessment, which is very important for the main population of shock – the elderly. The European society of Intensive Care Medicine states in consensus guidelines that echocardiography is recommended as the first choice for diagnosis and management regardless of whether the cause of shock is clear or not.[2]
Under handheld ultrasound scanning, physicians can quickly obtain information such as cardiac structure, ventricular function, and hemodynamic parameters to quickly identify the type and cause of shock. Four common types of shock include:
Cardiogenic shock
In the A4C view, the ejection fraction (EF value) is calculated according to the Simpson method to determine whether there is any disorder in left ventricular systolic function and observe color Doppler blood flow and color Doppler spectrum to check whether aortic aneurysm or aortic dissection occurs.
Hypovolemic shock
Observe whether the inferior vena cava changes with respiratory movement in the subxiphoid section, and measure the inferior vena cava dilatation index (dLVC). If dIVC>12%, it can be determined as insufficient volume.
Obstructive shock
Observe the presence of cardiac tamponade and pericardial effusion in the parasternal long-axis view. If the pressure in the pericardial cavity is greater than the pressure in the right atrium, it can be diagnosed as right atrial collapse and compression of the right ventricular outflow tract.
Distributive shock
Taking sepsis as an example, the stage and severity of the condition can be judged by observing the intensity of cardiac contraction and the amount of pleural effusion.
Point-of-care ultrasound in cardiorespiratory arrest (POCUS-CA)
Ultrasound is an important adjunct to cardiac arrest screening. According to the latest updated report from the American Heart Association in 2023:MI with OHCA or cardiac arrest in the ED occurred in 9682 (3.8%) of 252 882 patients from 224 hospitals in the NCDR ACTION Registry (2594 or 1.6% of patients with NSTEMI and 7088 or 7.5% of patients with STEMI).[3]
During the cardiac resuscitation stage, real-time images of the heart and the resuscitation rhythm are crucial to the doctor’s compression operation. Using handheld ultrasound can obtain real-time dynamic images of the heart to facilitate evaluation of the compression effect and reduce the impact on the resuscitation operation. Additionally, because quantitative capnography is less accurate in confirming endotracheal intubation in patients who have not returned spontaneous circulation, bedside cardiac ultrasound may be used for concurrent assessment.
TTE with Wireless Pocket Ultrasound
The application of echocardiography has expanded to a wider range of fields, such as evaluating the diastolic function of the patient’s heart, performing composite echocardiography, fetal echocardiography, vascular imaging, etc. At the same time, ultrasound equipment is getting smaller and smaller. The emergence of bedside echocardiography allows ultrasound to play a greater role in various departments. What originally required moving patients to the echocardiography room can now be completed at the bedside in the emergency room.
Common diseases in the emergency department usually involve the heart, lungs and abdomen. Common scans include goal or problem-directed ultrasonographic examination, focused assessment with sonography in trauma, (FAST), focused assessment of transthoracic echocardiography, FATE, or focused cardiac ultrasound (FCU). Viatom 3-in-1 handheld ultrasound is specially designed for emergency bedside cardiac scanning. The whole machine weighs 220g, which can be taken out of your pocket and used anytime and anywhere. It can be turned on in three seconds to quickly respond to emergency and severe scans. Viatom 3-in-1 handheld ultrasound C10 has built-in Wi-Fi to transmit high-definition images in real time so that physicians can seize the golden opportunity to save every minute and every second of the period.
Viatom C10 integrates linear array, convex array, and phased array into one. The sector-shaped low-frequency probe is 2.5-5Mhz (depth: 90~160mm). The highly penetrating phased probe is specially designed for cardiac structural evaluation; the convex array probe is 3.5-5Mhz (depth: 90~160mm). Depth: 90~305mm) is suitable for abdominal assessment and displays deep tissues; linear array probe 7.5-10Mhz (depth: 20~80mm) has high resolution and low penetration rate and is suitable for small organ and peripheral blood vessel examination.
Read more about Viatom C10 3 in 1 Wireless Pocket Ultrasound.
Conclusion
In the early application of imaging, physicians were limited by the limitations of a single environment and equipment volume and were unable to conduct diagnostic scans outside the department. With the development of small portable ultrasounds, portable, accurate, and non-invasive POCUs began to be used in more and more hospitals. Demonstrated promise of excellence in the clinical department. At present, the FOCUS has begun to undertake emergency medical rescue, immediate diagnosis of illness, and response to medical emergencies, effectively improving the uneven distribution of medical resources.
The American Society of Echocardiography pointed out in a consensus released in 2019 that physicians responsible for emergency echocardiography and routine echocardiography should receive long-term education and assessment, including current operational competency assessment and teaching training, and formulated emergency ultrasound training Guide for emergency echocardiography students and routine echocardiography students to learn and identify various possible cases to improve the quality of echocardiography and the efficiency of operations. At present, some medical schools in New York have distributed wireless ultrasound equipment to graduate students. The increased awareness of Pocus and the gradually standardized clinical skills will continue to support Pocus in supporting emergency medical diagnosis and providing personalized diagnosis and treatment plans.
Reference
[1]Scalea TM, Rodriguez A, Chiu WC, Brenneman FD, Fallon WF Jr, Kato K, McKenney MG, Nerlich ML, Ochsner MG, Yoshii H. Focused Assessment with Sonography for Trauma (FAST): results from an international consensus conference. J Trauma. 1999 Mar;46(3):466-72. doi: 10.1097/00005373-199903000-00022. PMID: 10088853.
[2]Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, Jaeschke R, Mebazaa A, Pinsky MR, Teboul JL, Vincent JL, Rhodes A. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med. 2014 Dec;40(12):1795-815. doi: 10.1007/s00134-014-3525-z. Epub 2014 Nov 13. PMID: 25392034; PMCID: PMC4239778.
[3]Tsao CW, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, Baker-Smith CM, Beaton AZ, Boehme AK, Buxton AE, Commodore-Mensah Y, Elkind MSV, Evenson KR, Eze-Nliam C, Fugar S, Generoso G, Heard DG, Hiremath S, Ho JE, Kalani R, Kazi DS, Ko D, Levine DA, Liu J, Ma J, Magnani JW, Michos ED, Mussolino ME, Navaneethan SD, Parikh NI, Poudel R, Rezk-Hanna M, Roth GA, Shah NS, St-Onge MP, Thacker EL, Virani SS, Voeks JH, Wang NY, Wong ND, Wong SS, Yaffe K, Martin SS; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2023 Update: A Report From the American Heart Association. Circulation. 2023 Feb 21;147(8):e93-e621. doi: 10.1161/CIR.0000000000001123. Epub 2023 Jan 25. Erratum in: Circulation. 2023 Feb 21;147(8):e622. Erratum in: Circulation. 2023 Jul 25;148(4):e4. PMID: 36695182.